Part 3 of 4
The Orphan Drug Act of 1983 and the Rare Diseases Act of 2002 were intended to reduce suffering by accelerating cures for rare conditions.
After more than four decades and billions in public spending, rare diseases have not diminished. They have multiplied—while an already bloated government spending program continues to expand, with no indication of an endpoint.
This is what has happened:
The Growth in Identified Rare Diseases
From just over 6,000 recognized in 2002, the count now exceeds 10,000 (per NIH, NORD, and Orphanet estimates as of 2025–2026), with new subtypes and classifications added yearly through advances in genetics, molecular diagnostics, and data aggregation. This outcome is not accidental; it is a feature of the current model.
Year | Estimated Number of Rare Diseases Identified |
2002 | ~6,000 |
2009 | ~5,850 |
2016 | ~6,080 |
2020 | ~7,000 |
2022 | ~10,000+ |
2026 | ~11,250+ (growing by ~250-300 annually) |
More labels translate to more patients identified, more protocols developed, and more lifelong management—not fewer people suffering. The economic burden reflects the same pattern: Rare diseases cost the U.S. nearly $1 trillion annually. Trillions are being spent collectively, yet meaningful reductions in prevalence or treatment dependency remain elusive. The overwhelming majority of rare diseases still have no cure; only about 5% have FDA-approved treatments.
Government Spending by Agency (Billions USD)
The increase in identified diseases correlates directly with massive increases in public spending, particularly on healthcare coverage (Medicare/Medicaid) as opposed to core research (NIH).
Year | NIH (Research) | FDA (Grants) | Medicare/Medicaid (Treatment) | Total Approx. |
2002 | ~$1.0B | $0.013B | Not Tracked | ~$1.01B+ |
2009 | $3.1B | $0.014B | ~$3.0B | ~$6.11B+ |
2016 | $4.9B | $0.016B | $10.0B | ~$14.92B+ |
2020 | $6.0B | $0.016B | $18.5B | ~$24.52B+ |
2022 | $7.2B | $0.017B | $27.1B | ~$34.32B+ |
2026 | $4.4B (Est.) | $0.019B | $33.0B (Est.) | ~$37.42B+ |
Activity vs. Progress
This outcome is by design. The system equates activity with progress: more grants awarded, more registries established, more approvals granted, more subtypes defined. Incentives reward participation and expansion—tax credits, market exclusivity, public-private collaborations—but impose no outcome-based accountability. There is no requirement to demonstrate fewer patients over time, fewer people needing lifelong therapy, or actual disease reduction. When prevalence rises or new diagnostic categories emerge, the funding continues unabated.
Regulatory flexibility, originally intended to address small patient populations, has granted pharmaceutical companies considerable leeway:
- Smaller Trials: Often involving only dozens of participants rather than thousands.
- Surrogate Endpoints: Using laboratory markers deemed “reasonably likely” to predict benefit, rather than direct evidence of clinical improvement like extended survival.
- Accelerated Approvals: Allowing initial marketing based on weaker data while post-approval confirmatory studies are frequently delayed or remain incomplete.
What began as exceptional accommodation has become routine, lowering evidentiary thresholds and enabling more drugs to reach the market with limited proof of resolving the underlying disease.
The Transparency Gap and Sidelined Interventions
Patients frequently receive incomplete information. While physicians must obtain informed consent, no federal rule mandates explicit disclosure that a drug is being used off-label, that supporting evidence derives from small trials or surrogate markers, or that long-term benefits and risks remain uncertain. This transparency gap places the full burden of uncertainty and potential harm squarely on the patient.
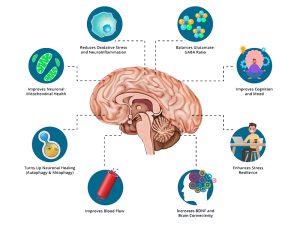
Non-patentable interventions—chronic infections, inflammatory drivers, environmental exposures, nutritional optimization, metabolic repair—are systematically sidelined. They lack the exclusivity or high-margin potential needed to attract large-scale funding or study. The system overwhelmingly favors scalable, reimbursable pharmaceutical solutions over investigation of root causes.
The human toll is profound and unforgivable. Patients endure aggressive, body-destroying regimens while underlying triggers go unexplored. They are told their disease is aggressive, rare, and incurable, then funneled into protocols designed for control rather than resolution.
What we really have created is a massive, well-funded, self-perpetuating industry: government-business partnerships, advocacy ecosystems, and lifelong treatment protocols—all thriving on more recognized diseases, more spending, and more dependency. Not progress. Institutionalized failure.
The next part begins at the moment a patient realizes they are not being guided toward recovery but managed as an endpoint in a system with no incentive to make them well—and decides to leave it.

Linda Wulf
Linda Wulf is a cancer rebel, advocate, and independent researcher. Diagnosed in 2023 with primary CNS lymphoma, she declined standard chemotherapy and pursued a root-cause, immune-supporting path. Twenty-three months cancer-free via root-cause approach.