Part 4 of 4
For the last three parts, we’ve traced how the Orphan Drug Act of 1983 started with genuine compassion, how the Rare Diseases Act of 2002 turned rare conditions into permanent federal infrastructure, and how the result is a trillion-dollar self-perpetuating industry that multiplies labels, inflates spending, and rewards management over cures. The system has no incentive to reduce disease prevalence, no requirement to prove fewer people need lifelong therapy, and no interest in exploring root causes when pharmaceutical control is more profitable.
What follows is real-world counter-evidence—one patient’s outcome that challenges the prevailing model. This is my story.
In late 2023, I was diagnosed with Primary CNS Lymphoma (PCNSL)—a “rare, aggressive, incurable” brain cancer. The standard protocol calls for high-dose methotrexate (HD-MTX), rituximab, temozolomide, and lifelong maintenance or repeated cycles of HD-MTX to keep this cancer from returning. If I was “lucky,” after 5-6 rounds, I’d qualify for an autologous stem cell transplant—harvesting my own cells to rebuild marrow destroyed by the chemo, all while the industry search for a “cure” drags on. A search first formalized in 1971 by Richard Nixon with the National Cancer Act, when he announced that if we can cure Hodgkin’s we can cure cancer.
At my doctor’s urging, I started HD-MTX just 10 days after landing in the ER—and a week after heavy antibiotics targeted what I believed was the real trigger: an active and chronic dental infection sparking my body’s lymphatic overreaction. While I was learning about the healthcare system and finding my way out, I went through four cycles of HD-MTX, and one dose each of rituximab and temozolomide.
By January 17, 2024, I’d gathered enough intel to plot my escape. Navigating my healthcare portal, I scrutinized my brain scans. What I saw didn’t scream “aggressive”—no rapid changes, just a body responding. It made more sense to challenge the story I was being told than to continue poisoning myself. I was learning in real time, unraveling rules and assumptions I wished I had known before the diagnosis. |
That day, admitted for what became my final cycle of HD-MTX, I refused anti-nausea meds. Vomiting, I argued, was my body’s natural defense against toxins—something it had done with cigarettes, alcohol, or even overwhelming experiences in my past. Why suppress that signal? Andrew Walker, the PA on shift, came in to talk. He listened thoughtfully as I shared my journey, my search for truth, and my question: Was it the antibiotics, the steroids or MTX driving any response? When he walked out that door, I expected to be shown the door—maybe even discharged from the program after he talked with the team.
Instead, he returned with “the Team” – Dr. Mrugala, Dr. Rosenthal, and others. The team couldn’t risk uncontrolled vomiting—I understood that. I told them plainly I believed my body could heal if I addressed the root cause. I said ” I am fearfully and wonderfully made.”
They listened, whether they heard me or were just nodding in agreement to get past this crisis. In my mind, I had just agreed to this last round, including anti-nausea for safety, on one condition: I’d head home to my octogenarian periodontist to tackle the infection. And that’s what I did. Looking back now, with everything I know, I would have left Mayo’s care on day 9—before ever starting chemotherapy. But fear and pressure kept me in longer than I should have stayed.
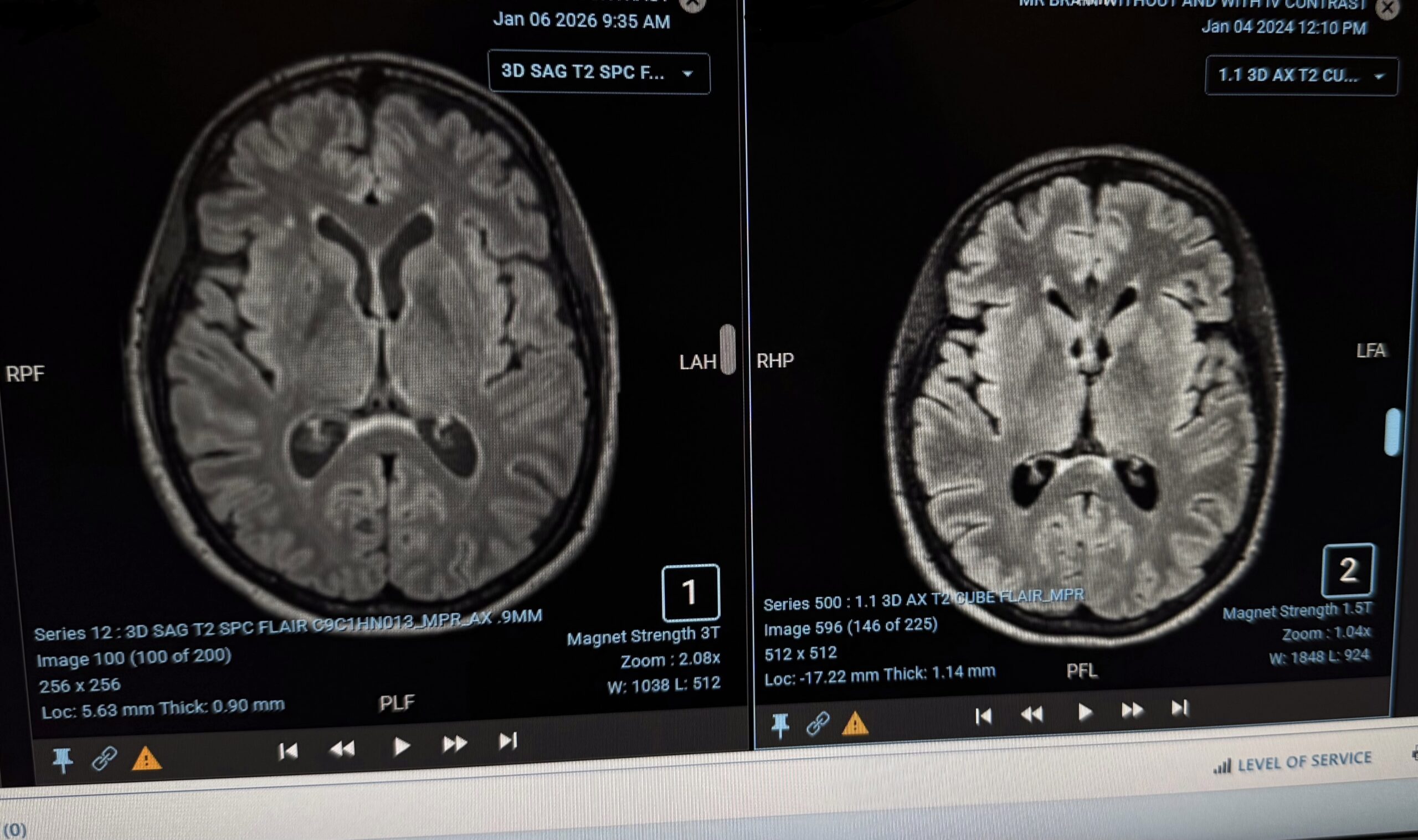
Fast-forward two years. My January 2026 MRI shows continued stability, with no new lesions and no meaningful progression of FLAIR hyperintensities. In the side-by-side comparison, the earlier scan (right) resembles a “lion’s face,” its mane formed by flaring abnormalities around the brain’s center. In the most recent image (left), those features appear subdued and organized—the central structures tamed, the brain moving from roaring to resting.
On January 19, 2026, I returned to my doctor, and we reviewed the imaging. We agreed that I would permanently step away from Mayo Clinic’s monitoring of my “disease.” There was no fanfare when I walked out—no longer their patient. No one is ringing my “I beat cancer” bell but me.
I am no longer living on borrowed time. I am living on healing on my terms—without endless toxicity.
- The system is structured around features that are rarely disclosed to patients. These are the priorities and mechanisms I wish I had understood earlier:Drugs are prioritized over whole-body health. Medical care often follows rigid treatment playbooks that focus on pharmaceuticals, and once those regiments are established, they are rarely questioned or revisited.
- Suppression replaces biological support. Rather than helping the body’s natural defense systems do their job, many treatments are designed to shut them down—most notably by targeting the lymphatic and immune systems first, even as they are actively working to protect and stabilize the body.
- Approvals continue without ongoing proof. Once a drug is approved, it can remain in use indefinitely, even when long-term effectiveness is not regularly re-evaluated or meaningfully tracked.
- Rules are bent for labels, not outcomes. Regulatory flexibility around “rare” disease classifications serve faster approvals and bureaucratic objectives rather than ensuring real, patient-centered results.
- Important gaps are left uncovered. Insurance routinely excludes testing that could explain ongoing symptoms—such as evaluations for gadolinium toxicity—simply because those tests fall outside standard pathways.
- Drugs gain freedom, patients do not. After approval for a single cancer indication, drugs can be reused broadly in small patient groups without rigorous endpoints, long-term follow-up, or meaningful outcome tracking.
- Treatment rules are shaped by industry. Pharmaceutical companies develop the drugs, influence testing, and help shape hospital protocols—often through industry-entangled organizations like National Comprehensive Cancer Network—aligning care more closely with profit and stock performance than with patients’ long-term well-being.
- Language is used to narrow choices. Fear-based terms like “aggressive,” “incurable,” and “unbeatable” are routinely used to frame disease, discouraging questions and implying patient helplessness rather than describing biological reality.
- Patients are kept in a treatment loop. Most are never told that stopping, monitoring, or supporting the body is an option, ensuring continued enrollment in regiments that sustain dependency, funding streams, registries, and repeat interventions instead of resolution.
My message to anyone reading this series: You are not a disease label. Your body is remarkable. When the protocol feels like destruction, question it. Seek second opinions. Trust your intuition. Explore nutrition, detoxification, inflammation reduction, and lifestyle—the things the system sidelines because they can’t be patented or scaled. Healing is possible. Freedom is possible.
The industry we have created thrives on dependency. But individuals can break free—and when we do, we prove the whole narrative wrong.

Linda Wulf
Linda Wulf is a cancer rebel, advocate, and independent researcher. Diagnosed in 2023 with primary CNS lymphoma, she declined standard chemotherapy and pursued a root-cause, immune-supporting path. Twenty-three months cancer-free via root-cause approach.